July 5, 2025 Story by: Editor
A Columbia University study projects a sharp rise in uterine cancer cases and deaths in the United States over the next 25 years, with Black women facing the most severe increases. Utilizing a comprehensive model that accounts for age, race, cancer subtype, obesity trends and hysterectomy rates, researchers caution that if current patterns persist, public health outcomes could worsen substantially.
To predict future trends in uterine cancer incidence and mortality, researchers at Columbia built a natural history model that allowed them to simulate the trajectories of women over time based on age, type of uterine cancer, and race. Survival estimates are based on currently available treatments. The model also includes current rates of obesity, a known risk factor for uterine cancer, and hysterectomy, which reduces the risk.
“Our model predicts that current trends in uterine cancer incidence and mortality will continue for the foreseeable future,” says the study’s first author, Jason D. Wright, the Sol Goldman Professor of Gynecologic Oncology at Columbia University Vagelos College of Physicians and Surgeons. “From 2018 to 2050, we expect uterine cancer cases to rise by over 50% in Black women versus about 29% in white women.”
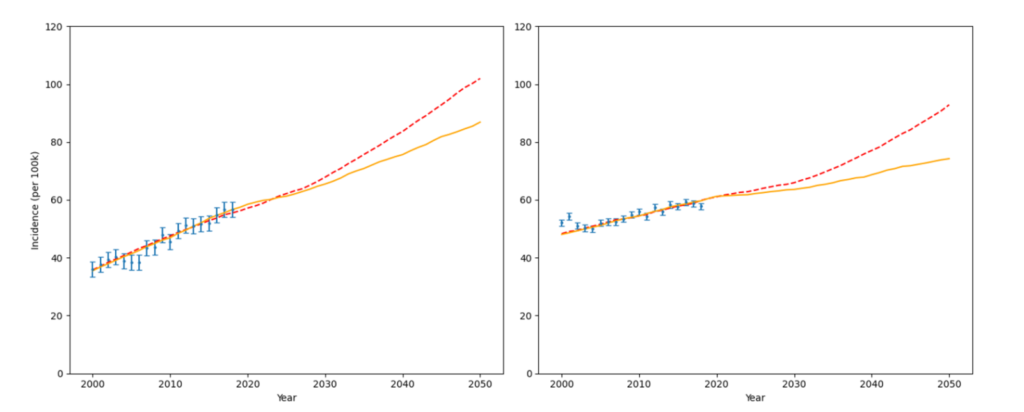
Photo caption: Rising rates of uterine cancer. The Columbia University Uterine Cancer Model predicts uterine cancer rates will continue to rise in the next 25 years for both Black (left) and white (right) women. The dashed line represents the predicted rise if obesity and hysterectomy rates continue to rise and fall, respectively. The orange line represents the predicted rise if obesity and hysterectomy rates do not change from today’s rates. (Photo courtesy of Columbia University Irving Medical Center)
The model closely fit population-based incidence and mortality data of uterine cancer. From 2020 to 2050, the incidence of uterine cancer is projected to increase in White women to 74.2 cases per 100,000 (compared with 57.7 cases per 100,000 in 2018) and increase to 86.9 per 100,000 (compared with 56.8 cases per 100,000 in 2018) in Black women.
Among White women, incidence-based mortality will increase from 6.1 per 100,000 in 2018 to 11.2 per 100,000 in 2050, whereas incidence-based mortality in Black women will increase from 14.1 per 100,000 to 27.9 per 100,000.
Endometrioid tumors are expected to increase considerably in both White and Black women; White women will experience only a slight increase in nonendometrioid tumors, whereas the incidence of these tumors will increase substantially in Black women.
The overall five-year survival rate for Caucasian women with uterine cancer is 84% versus 63% for African American women. This cancer is slightly more common in African American women, and they are more likely to die from it than Caucasian women.
Key Findings
Soaring incidence rates
- Among Black women, cases of uterine cancer are projected to rise from 56.8 to 86.9 per 100,000 between 2018 and 2050—a 53% increase.
- For white women, cases are expected to increase from 57.7 to 74.2 per 100,000, marking a 29% rise.
Rising mortality
- Deaths among Black women could nearly double, increasing from 14.1 to 27.9 per 100,000.
- Among white women, deaths may climb from 6.1 to 11.2 per 100,000.
Drivers of disparity:
- Black women are more frequently diagnosed with aggressive non-endometrioid subtypes and face delays in diagnosis and treatment.
- Systemic factors—such as healthcare access, socioeconomic inequities, and potentially harmful exposures (like certain cosmetic chemicals)—likely exacerbate these outcomes.
Why Rates Are Rising
- Population aging and an obesity epidemic fuel higher incidence—both well-established risk factors for uterine cancer.
- Declining hysterectomy rates—owing to less surgical intervention for benign conditions—mean more women remain at risk for developing cancer.
- A notable rise in aggressive non-endometrioid tumors, especially in Black women, is driving both incidence and mortality upward.
Screening, Treatment & Prevention
Currently, there is no routine screening for asymptomatic uterine cancer. Detection relies on transvaginal ultrasound and endometrial biopsy if symptoms like abnormal bleeding arise.
However, the Columbia model suggests that introducing a screening tool at age 55 could reduce incidence by up to 15–16 years in both Black and white populations, demonstrating the potential impact of earlier detection.
Call to Action
- Developing effective screening programs is urgent, especially targeting high-risk groups and asymptomatic individuals.
- Public health efforts should tackle underlying risk factors—focusing on obesity prevention and timely healthcare access.
- Policy interventions and education are critical to dismantle barriers hindering early diagnosis and culturally responsive care.
Looking Ahead
This study underscores uterine cancer as one of the few malignancies with rising incidence and mortality—and highlights growing racial disparities in outcomes. It places Black women at the center of concern: they will face the steepest increases unless meaningful intervention occurs.
As Dr. Jason D. Wright, the study’s lead author, emphasizes: “Our findings underscore the urgent need to develop new strategies to prevent and screen for uterine cancer in high-risk women”.
The projections presented serve as a wake-up call—pointing to a critical moment for cancer prevention, equity in care delivery, and innovation in diagnostic strategies.
Source: Columbia University Irving Medical Center / Inside Precision Medicine / The National Foundation for Cancer Research